Dealing with Mallet Finger can be an uncomfortable and disruptive experience, often accompanied by pain and functional limitations. Imagine the frustration of struggling to straighten your finger, perform daily tasks like gripping objects or typing, and even simple actions like buttoning a shirt. Mallet Finger can indeed impact your quality of life, making it essential to seek the right care and expertise to address this condition effectively.
At the Sydney Orthopaedic Surgeon Clinic, we have an intimate understanding of the challenges that Mallet Finger poses. Led by the experienced orthopaedic surgeon and upper limb specialist, Dr Stuart Kirkham, our team is dedicated to providing tailored and compassionate care to individuals facing this condition. Dr Kirkham’s extensive expertise in orthopaedics ensures that you receive personalised treatment that suits your unique needs.
Whether your Mallet Finger is a minor inconvenience or requires surgical intervention, Dr Kirkham has the expertise to offer a range of treatment options. His non-surgical approaches include methods like splinting, pain management, and wound care, aimed at promoting healing and minimising discomfort. For more severe cases, Dr Kirkham opts for surgical treatments such as the Kirschner wire fixation, designed to restore function and prevent complications.
If you’re concerned about your Mallet Finger and its impact on your life, we encourage you to take the first step toward recovery. Reach out to Dr Kirkham today and schedule a consultation at one of his five conveniently located modern clinics across the Sydney region. With his experience, commitment and expertise, you can regain control over your daily activities and overall quality of life with a comprehensive treatment plan tailored to your needs.
Anatomy Affected by Mallet Finger
Mallet Finger, also known as “baseball finger” or “drop finger,” is a condition that occurs when the extensor tendon at the distal interphalangeal joint (DIP joint) of the finger is injured or torn. To understand this condition better, let’s take a closer look at the anatomy of the finger.
Your finger is an intricate assembly of bones, tendons, and joints that work harmoniously to allow for dexterity and movement. At the heart of the Mallet Finger lies the DIP joint, which is the last joint of the finger, located just before the fingertip. The DIP joint plays a crucial role in finger extension, allowing you to straighten your finger and perform various activities that require precision and strength.
The extensor tendons, on the other hand, are the tough, fibrous structures that connect muscles to bones. In the context of Mallet Finger, these tendons are responsible for extending your finger at the DIP joint. When these tendons are damaged due to trauma or injury, it disrupts the delicate balance required for smooth finger movement.
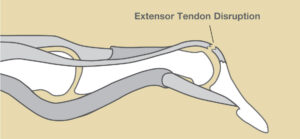
Imagine your finger as a well-coordinated puppet, with the DIP joint acting as the string that pulls it straight. The extensor tendons may be seen as the puppeteer’s strings. They contract and relax in response to muscle movement, allowing your finger to bend and extend. However, when an injury occurs at the DIP joint, such as in Mallet Finger, it’s like cutting one of those strings. The result is an inability to fully extend the finger, leading to the characteristic drooping or “mallet” appearance.
Understanding the anatomy behind Mallet Finger is crucial in recognising the source of the condition and understanding the limitations it can impose. If you suspect you may be experiencing symptoms of Mallet Finger or have any concerns about your finger’s anatomy, don’t hesitate to reach out to Dr Kirkham. A thorough examination can provide Dr Kirkham with valuable insights into how Mallet Finger may be impacting your finger’s intricate structure. Don’t let this condition limit your finger’s potential – take the first step towards recovery and better finger function by scheduling a consultation with Dr Kirkham today. Your finger’s well-being is our priority.
Causes and Risk Factors for Mallet Finger
Mallet Finger is caused by an injury to the extensor tendon, which sits at the top of the finger and allows it to straighten. However, there are two different types of injuries to the area that can result in an individual developing Mallet Finger.
The first type of Mallet Finger occurs due to an injury to the extensor tendon itself, and this is often referred to as a rupture. This injury can occur as a result of jamming or cutting the finger. It can also develop slowly over time, particularly in cases where arthritis leads to the gradual stretching of the tendon. In essence, this type of Mallet Finger is a consequence of the extensor tendon losing its integrity, affecting its ability to effectively straighten the finger.
The second type of Mallet Finger arises from a fracture at the site where the extensor tendon attaches to the bone. In this case, the tendon itself remains intact, but the bone to which it is anchored breaks off. This particular type of Mallet Finger is sometimes observed in children, where the fracture can occur in the growth plate of the distal phalanx.

Certain traumatic incidents, such as when an object forcefully strikes the tip of the finger or thumb (which is common in baseball), can lead to either a tendon injury or a broken-bone type of Mallet Finger, earning it the colloquial name, baseball finger. However, Mallet Finger may instead be the result of forceful bending of the joint during activities like lifting heavy objects that force the joint into a bent position. Sometimes, even minor force applied at an awkward angle can lead to tendon rupture. Everyday actions such as scrubbing dishes or accidentally bumping an object while putting clothes into a drawer can contribute to this condition.
If you suspect you may be suffering from Mallet Finger or have experienced any of these causes, consult with Dr Kirkham for a thorough evaluation. His expertise can provide insights into your specific case and guide you towards the most appropriate treatment and management options. Don’t let Mallet Finger hold you back – take the first step towards recovery by reaching out to Dr Kirkham for his personalised care and support.
Symptoms and Identification of Mallet Finger
Recognising the presence of Mallet Finger is generally not a difficult task given the deformity that it often causes, but it may be confused with other similar conditions. However, it does feature some distinctive symptoms which can be both primary and secondary in nature.
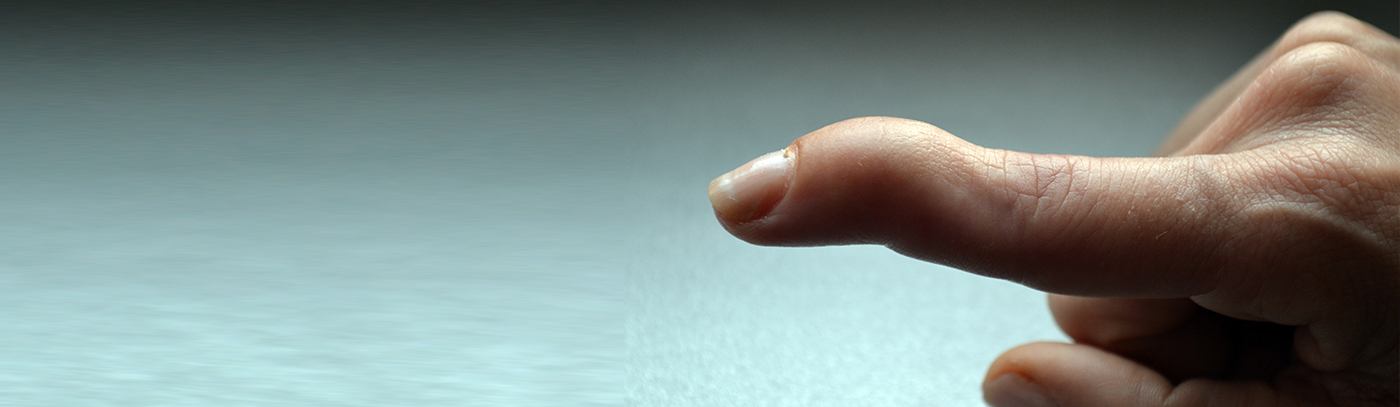
The primary symptom of Mallet Finger is the noticeable drooping of the fingertip, often accompanied by redness under the fingernail. This drooping occurs because the extensor tendon, responsible for straightening the finger, has been injured. As a result, the fingertip remains in a bent position, resembling the shape of a mallet, hence the condition’s name.
Beyond this highly visible change, individuals with Mallet Finger may experience an inability to straighten the affected finger fully. This limitation in finger movement can significantly impact daily activities, from typing on a keyboard to grasping objects, and even performing routine tasks like buttoning a shirt.
Less overt symptoms of Mallet Finger may include pain, swelling, and bruising. The pain can vary in intensity, from mild to severe, and is typically localised to the injured finger. Swelling and bruising result from the body’s natural response to injury and may further contribute to discomfort and visual changes in the affected area.
Distinguishing Mallet Finger from similar injuries, such as a simple finger sprain or strain, is essential for accurate diagnosis and prompt treatment. While sprains and strains may share some symptoms with Mallet Finger, the characteristic drooping of the fingertip sets Mallet Finger apart.
If you suspect that you’ve developed Mallet Finger based on these symptoms or if you’re unsure about the nature of your finger injury, it’s advisable to seek the advice of Dr Kirkham. Your consultation with Dr Kirkham can provide a definitive diagnosis, allowing for timely intervention and a tailored treatment plan to address your specific condition, setting you on course for a smooth recovery.
Diagnosis and Imaging of Mallet Finger
Diagnosing Mallet Finger requires a comprehensive approach that combines clinical examination and imaging techniques. Dr Kirkham employs a thorough clinical examination method to assess the finger’s condition. During this physical examination, he carefully evaluates the injured finger, paying close attention to the extent of drooping, the extent to which the finger can be straightened and extended, and any other associated symptoms. This hands-on assessment allows him to gauge the severity of the Mallet Finger and determine the most suitable course of action.
In addition to the clinical examination, imaging techniques play a vital role in confirming the diagnosis and ruling out potential fractures or soft tissue injuries. X-rays are almost always used to evaluate and diagnose Mallet Finger. They provide detailed images of the bone structures and can help identify any fractures or dislocations in the affected area. By using X-rays, Dr Kirkham can ensure that no underlying bone damage exists, which may require specific interventions.

In rare cases where soft tissue evaluation is required, an MRI or Ultrasound may be conducted to provide a more in-depth examination of the soft tissues, including tendons and ligaments, providing valuable insights into the extent of the injury.
Early diagnosis is of paramount importance when dealing with Mallet Finger. Detecting and addressing the condition promptly can help prevent long-term complications and ensure a more favourable outcome. Timely treatment can often lead to a quicker and more complete recovery, minimising the risk of joint stiffness, deformity, or chronic pain that can result from untreated or inadequately managed Mallet Finger.
Should you suffer from the symptoms of Mallet Finger, Dr Kirkham is always ready to assist you at any of his 5 Sydney Orthopaedic Surgeon clinics. With his expertise in the diagnosis and treatment of hand and finger injuries, Dr Kirkham is the ideal choice for a thorough evaluation. Don’t let uncertainty about your finger’s condition linger – reach out to Dr Kirkham for a precise diagnosis and personalised treatment plan tailored to your specific needs.
Treatment Options for Mallet Finger
When it comes to treating Mallet Finger, there are both non-surgical and surgical options available, each tailored to the severity of the condition.
For milder cases of Mallet Finger, non-surgical approaches can often yield successful results. One of the primary non-surgical treatments is splinting for a number of weeks to hold the fingertip in an extended position, allowing the damaged extensor tendon to heal properly. The duration of splinting can vary but typically lasts for several weeks to ensure the tendon heals adequately.
Physical therapy can also play a significant role in non-surgical treatment. It involves exercises and techniques aimed at improving finger mobility and strength. Physical therapy can complement splinting, helping restore normal finger function and prevent stiffness.
In more severe cases of Mallet Finger, surgical intervention may be necessary to restore finger function fully. Surgical options include tendon repair, Kirschner wire fixation, and open reduction internal fixation.
Tendon repair involves reattaching the damaged extensor tendon to its original position. This surgical procedure aims to restore the finger’s ability to extend fully and effectively. Alternatively, a Kirschner wire fixation may be used, which involves the insertion of a wire to stabilise the joint and maintain proper alignment during the healing process. This technique is typically reserved for cases related to a fracture where a reconstruction is required. Open reduction internal fixation is a surgical approach reserved for tendinous Mallet Finger where the tendon requires a repairing surgery.
Dr Kirkham has great experience delivering each of these surgeries and will work closely with you to determine the best approach for your specific case. Don’t hesitate to reach out to Dr Kirkham for expert guidance on your path to recovery with an initial consultation at any of his Sydney clinics.
Prevention and Aftercare for Mallet Finger
Preventing Mallet Finger can be challenging, as accidents can happen unexpectedly. However, there are some preventive measures that can reduce the risk, particularly in high-risk scenarios. In sports, wearing protective gear like finger splints or guards can provide added protection to the fingers, reducing the likelihood of injury. Similarly, in high-risk occupations involving manual labour or activities that strain the fingers, following safety protocols and using protective equipment can help minimise the chances of Mallet Finger occurring.
Aftercare plays a vital role in the recovery process for Mallet Finger. Following the prescribed treatment plan diligently is crucial to promote proper healing and prevent complications. This may include wearing splints as directed, attending physical therapy sessions, taking any prescribed medications or following wound care instructions. Consistency in aftercare can significantly impact the speed and success of recovery.
Rehabilitation exercises are often an integral part of aftercare for Mallet Finger. These exercises aim to improve finger mobility and strength, helping individuals regain full function and prevent stiffness. Engaging in these exercises as advised by a healthcare professional is essential for a successful recovery.
At the Sydney Orthopaedic Surgeon Clinic, Dr Kirkham and his dedicated team are well-equipped to provide comprehensive aftercare for Mallet Finger. If you’ve experienced a Mallet Finger injury and are seeking effective aftercare, reach out to Dr Kirkham for specialised care tailored to your specific needs. Your finger’s well-being is our priority, and we are here to support your journey to recovery and ensure you can confidently return to your daily activities.
The Recovery Process from Mallet Finger
Understanding the possible complications of Mallet Finger is crucial for making informed decisions and understanding what to expect from your recovery. The recovery timeline for Mallet Finger can vary based on whether non-surgical or surgical treatments are employed. Non-surgical approaches often require several weeks of splinting and physical therapy to promote healing and restore function. Surgical treatments may involve a more extended recovery period, and the specific timeline can vary depending on the complexity of the procedure and the severity of the condition.
Milestones in the recovery process are important markers of progress. Patients can anticipate a reduction in pain as the injured finger heals and inflammation subsides. Improved mobility and strength will gradually follow, allowing for a phased return to normal activities. While it’s important to remember no two recovery periods are exactly alike, patience and commitment to the prescribed treatment plan often prove vital in ensuring a swift recovery is experienced.
If you or someone you know is dealing with Mallet Finger or has concerns about the recovery process, consulting Dr Kirkham is the best course of action. His expertise in hand and finger injuries ensures that you receive the appropriate guidance and support throughout your recovery journey. Don’t hesitate to reach out to Dr Kirkham to discuss your specific situation and receive individualised care to help you achieve the best possible outcome.
Possible Complications of Mallet Finger
Common complications that individuals may encounter during their recovery include joint stiffness, deformity, and chronic pain. Joint stiffness can result from prolonged immobilisation or inadequate rehabilitation. Deformity may occur if the condition is not adequately treated, leading to a permanent misalignment of the affected finger. Chronic pain can persist if underlying issues, such as joint damage or residual inflammation, are not addressed.
Infection following any form of surgery is a possibility, albeit extremely unlikely, especially under the expertise of Dr Kirkham. Ensuring proper wound care and following post-operative instructions can significantly reduce this risk. Another rare occurrence to note is tendon necrosis, which involves the death of tendon tissue and may require further intervention.
Mitigating these complications begins with prompt and appropriate treatment. Early diagnosis and suitable interventions, whether surgical or non-surgical, can prevent many complications. Additionally, adhering to the recommended aftercare plan, including physical therapy and lifestyle modifications, can help mitigate joint stiffness, deformity, and chronic pain. Proper wound care and vigilant monitoring are essential to minimise the risk of infection post-surgery.
With diligent care and adherence to medical advice, most individuals can expect a successful recovery from Mallet Finger. Consulting Dr Kirkham is an important step to ensure you receive expert guidance and minimise the potential for complications. If you have any concerns about your Mallet Finger recovery or are experiencing complications, don’t hesitate to reach out to Dr Kirkham at any point in your recovery process.
Are You Concerned About Mallet Finger?
If you’re worried about a Mallet Finger injury, it’s important to recognise that you’re not alone, and we’re here to help. Mallet finger injuries can be uncomfortable and concerning, but seeking timely medical attention is crucial. Without proper care, these injuries can lead to complications that affect your hand’s function.
Dr Kirkham and his team of dedicated professionals at the Sydney Orthopaedic Surgeon Clinic understand the challenges you may be facing. Whether you’re experiencing mild discomfort or severe pain with difficulty in finger movement, we are here to provide the expert care you need.
Your concerns about mallet finger are valid, and we encourage you not to endure them silently. Contact us today to arrange a consultation with Dr Kirkham and take the first step toward improving your hand’s mobility, reducing pain, and enhancing your quality of life. He will conduct a thorough assessment and create a customised treatment plan tailored to your specific needs and condition. Your well-being is his priority, and Dr Kirkham is ready to support you every step of the way, from diagnosis to aftercare.
FAQs
1. Can I leave mallet finger untreated?
Leaving mallet finger untreated is not advisable due to the potential complications it can lead to. Mallet finger disrupts the balance of extensor force in the finger joints, potentially causing a swan neck deformity. This deformity involves hyperextension of the proximal interphalangeal (PIP) joint and flexion of the distal interphalangeal (DIP) joint, which can affect both function and appearance. Seeking prompt medical attention and appropriate treatment, such as splinting, is crucial to prevent these long-term issues and ensure a smoother recovery.
2. How long do I need to wear a splint to treat mallet finger?
Continuous splinting is essential for mallet finger treatment to achieve optimal results. The splint should not be removed for any activities, including washing or showering. Typically, you will need to wear the splint full-time for a minimum of eight weeks, followed by an additional two weeks for protective activities. However, it’s important to note that the splinting duration may vary depending on individual factors and the presence of any complications. Your healthcare provider will provide guidance specific to your case.
3. Is surgery always necessary for Mallet Finger?
Surgery is not always required for mallet finger. Immediate medical attention is crucial if there’s an open wound or bleeding associated with the injury. Surgery may be considered if there’s a significant or displaced fracture of the finger. However, in cases where there is no fracture, conservative treatment involving splinting the finger in a straight position may be sufficient. It’s essential to have your condition properly evaluated by a hand surgeon to determine the most suitable treatment approach for your specific circumstances.
4. How do you know if mallet finger has healed fully?
Determining whether mallet finger has fully healed involves several factors. One indicator that healing may not be complete is the presence of swelling in the finger when the splint is no longer worn. This can be a sign that the tendon has not healed adequately. In such cases, additional evaluation, including another x-ray, may be necessary to assess the progress of healing. If your finger has not fully healed by the end of the initial treatment period, your healthcare provider may recommend an additional four weeks of wearing the splint to support the healing process and ensure the best possible outcome.
5. Will the finger look normal after the injury?
Most mallet finger injuries recover full function, but there may be some residual effects. The tip of the finger may remain slightly thicker than before the injury. Additionally, there could be a slight limitation in movement, with the finger not fully straightening or bending as it did previously. However, these effects are typically minimal, and with appropriate treatment and rehabilitation, the finger can regain both functional and cosmetic normalcy. The focus is on restoring the best possible hand function while minimising any lasting cosmetic changes. Your healthcare provider can provide guidance on managing and addressing these concerns during your recovery process.
References
- American Society For Surgery of the Hand (Mallet Finger: Symptoms & Treatment)
- OrthoInfo (Mallet Finger)
- Cleveland Clinic (Mallet Finger)
- NHS (Mallet Finger)